Research & Articles
I am passionate about educating the next generation of Medical Students and Future Doctors, particularly inspiring them to pursue a career in Orthopaedic Surgery. With the rise of Virtual Reality and Simulation Training, Robotic Surgery and Artificial Intelligence, it is a fascinating and exciting time to be in Surgical Education and Research.
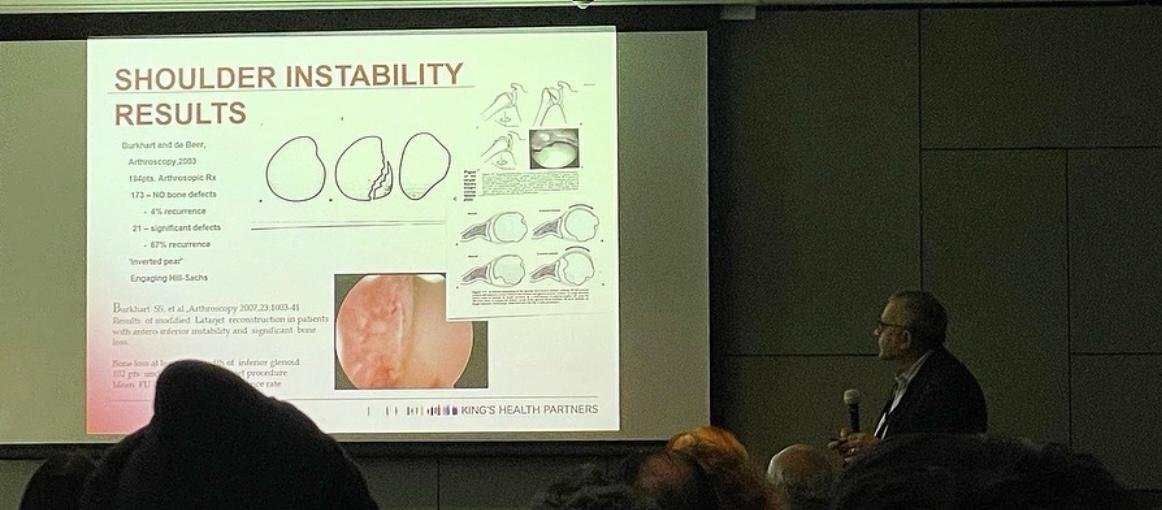
Throughout my career, I have continued teaching both Medical Students and Post-Graduate Students and I am an Honorary Senior Lecturer at Kings College London. I am actively involved in Kings Health Partners (KHP), both as a joint CAG (Clinical Academic Group) Leader for Orthopaedics, Trauma and Plastics, and actively involved in KHP Academic Surgery.
Artificial intelligence in orthopaedic surgery: transforming technological innovation in patient care and surgical training.
St Mart,J-P, Goh,EL, Liew,I, Shah,Z, Sinha,J.
Postgrad Med J,2022,April.
DOI: 10.1136/postgradmedj-2022-141596
https://academic.oup.com/pmj/article/99/1173/687/7211549?login=false
Abstract
Artificial intelligence (AI) is an exciting field combining computer science with robust data sets to facilitate problem-solving. It has the potential to transform education, practice and delivery of healthcare especially in orthopaedics. This review article outlines some of the already used AI pathways as well as recent technological advances in orthopaedics. Additionally, this article further explains how potentially these two entities could be combined in the future to improve surgical education, training and ultimately patient care and outcomes.
Keywords: hip; knee; medical education & training; orthopaedic & trauma surgery.
The Effect of the COVID-19 Pandemic on Mental Health Associated Trauma, Admissions and Fractures at a London Major Trauma Centre
M S Jamal, D Hay, K Al-Tawil, A Petohazi, V Gulli, N Bednarczuk, R Baldwin-Smith, J Gibbons, J Sinha
British Journal of Surgery, Volume 108, Issue Supplement_6, September 2021, znab259.979,
https://doi.org/10.1093/bjs/znab259.979
Abstract
Aim
Non-injury related factors have been extensively studied in major trauma and shown to have a significant impact on patient outcomes, with mental illness and associated medication use proven to have a negative effect on bone health and fracture healing. We report the epidemiological effect of COVID-19 pandemic on mental health associated Orthopaedic trauma, fractures, and admissions to our centre.
Method
We collated data retrospectively from the electronic records of Orthopaedic inpatients in an 8-week non-COVID and COVID period analysing demographic data, referral and admission numbers, orthopaedic injuries, surgery performed and patient co-morbidities including psychiatric history.
Results
here were 824 Orthopaedic referrals and 358 admissions (6/day) in the non-COVID period with 38/358 (10.6%) admissions having a psychiatric diagnosis and 30/358 (8.4%) also having a fracture. This was compared to 473 referrals and 195 admissions (3/day) in the COVID period with 73/195 (37.4%) admissions having a documented psychiatric diagnosis and 47/195 (24.1%) a fracture. 22/38 (57.9%) and 52/73 (71.2%) patients were known to mental health services, respectively.
Conclusions
Whilst total numbers utilising the Orthopaedic service decreased, the impact of the pandemic and lockdown disproportionately affected those with mental health problems, a group already at higher risk of poorer functional outcomes and non-union. The proportion of patients with both a fracture and a psychiatric diagnosis more than doubled and the number of patients presenting due to a traumatic suicide attempt almost tripled. It is imperative that adequate support is in place for vulnerable mental health patients, particularly as we are currently experiencing the “second wave” of COVID-19.
Value-based healthcare analysis of shoulder surgery for patients with symptomatic rotator cuff tears – Calculating the impact of arthroscopic cuff repair
C Holzer-Fleming, A Tavakkolizadeh, J Sinha, J Casey, J Moxham, Toby J Colegate-Stone
2020 Jul 2;14(1 Suppl):59–70. doi: 10.1177/1758573220928258
Abstract
Background
Surgical repair of full-thickness rotator cuff tears in symptomatic patients is known to offer significant benefits. Despite this there remains a lack of universal appreciation that such surgery offers high clinical value, with some commissioners even limiting access to it. The value-based healthcare agenda provides a means to design, deliver and measure the impact of healthcare to a defined segment of patients. The aim of this study was to measure the value of surgically repairing primary symptomatic full-thickness rotator cuff tears when outcomes and costs were assessed over an entire care pathway.
Methods
A prospective study of patients undergoing rotator cuff tears repair was undertaken. Patients were managed using a standardised integrated care pathway. Subsequent outcomes and costs were measured over the whole care pathway. Outcomes were assessed from both traditional and patient centric re-formatted prisms.
Results
Significant improvement in clinical outcomes where recognised when assessed from either the traditional or re-formatted prisms. Economic review of this approach revealed the pathway generated a sustainable and notable positive margin.
Discussion
This study evidences how a well-designed value-based healthcare shoulder approach can be delivered and measured. It demonstrates rotator cuff surgery to be a high value treatment for patients with symptomatic rotator cuff tears.
Keywords: Rotator cuff repair, value-based healthcare, outcomes
Robotics in trauma and orthopaedics
Karthik Karuppiah 1, Joydeep Sinha 2
Ann R Coll Surg Engl. 2018 May 2;100(6 sup):8–18.
Abstract
Recent advances and review of literature.
Robot-assisted orthopaedic surgery is gaining momentum and being gradually adopted and incorporated into our routine practice. With recent innovations in surgical applications of robots, newer techniques are developed and its applications rapidly expanding in orthopaedics. This article reviews the current state of robotics and the development of future robotic technology for Trauma and Orthopaedics.
Increasing value: The King's College Hospital Experience
Toby Colegate-Stone, Adel Tavokkolizadeh, John Moxham, Joydeep Sinha
British Journal of Healthcare ManagementVol. 22, No. 6
Published Online:21 Jun 2016. https://doi.org/10.12968/bjhc.2016.22.6.326
Abstract
The increasing trauma demands imposed by our population require innovative practice. A day surgery trauma service is a pragmatic response for those patients with less severe, more ambulatory trauma, and whose surgery has a lower risk profile. By using the principles set out in the value-based healthcare (VBHC) agenda, such a re-orientation of service offers opportunities in improving outcomes and reducing costs, this study assessed the impact of the day surgery trauma service in its current activity, the outcomes generated, its potential development and its fiscal footprint. The average patient satisfaction was very good with 92% preferring their surgery performed as day surgery rather than as an inpatient. Day surgery was noted to have a higher run rate of cases per unit of time, lower costs and subsequently a better margin generation per minute. The additional annual profit generated by performing a single whole day trauma list in day surgery was approximately £293 000. By focusing on the needs of the patients and placing them at the centre of service re-design constructive change is seen to be possible. The day surgery trauma service can be shown to deliver higher value care. Triaging the locus of surgery in this way helps to get patients to the best place for the best outcome.
Robotic surgery in trauma and orthopaedics: a systematic review
K Karthik, T Colegate-Stone, P Dasgupta, A Tavakkolizadeh, J Sinha
Bone Joint J. 2015 Mar;97-B(3):292-9.
doi: 10.1302/0301-620X.97B3.35107
Abstract
The use of robots in orthopaedic surgery is an emerging field that is gaining momentum. It has the potential for significant improvements in surgical planning, accuracy of component implantation and patient safety. Advocates of robot-assisted systems describe better patient outcomes through improved pre-operative planning and enhanced execution of surgery. However, costs, limited availability, a lack of evidence regarding the efficiency and safety of such systems and an absence of long-term high-impact studies have restricted the widespread implementation of these systems. We have reviewed the literature on the efficacy, safety and current understanding of the use of robotics in orthopaedics.
Keywords: robotics; haptics; bone; orthopaedics; orthopaedic surgery; trauma; arthroplasty; arthroscopy.



